Arthritis: Foods to Eat and Foods to Avoid (Evidence Based)
Many diseases, including arthritis are caused by chronic low-grade inflammation. It is now widely accepted that some foods fuel inflammation, while others make it better. Foods like extra virgin olive oil, coconut oil, and fatty fish are scientifically proven to reduce inflammation and improve the symptoms of arthritis. Medical studies have also revealed that supplements like glucosamine and chondroitin can be effective in treating osteoarthritis.
In this article I am going to cover foods and supplements that are scientifically proven to improve symptoms of Osteoarthritis (OA) and Rheumatoid arthritis (RA). At the end of the article I’ll cover the connection between vitamin D and Rheumatoid arthritis (RA).
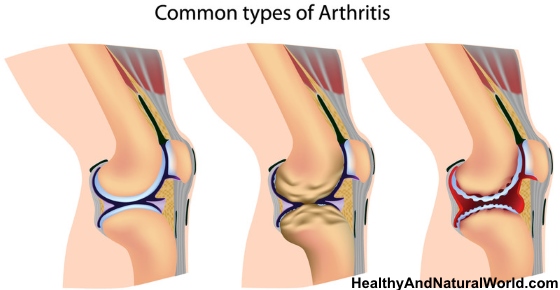
Types of Arthritis
It’s important to distinguish between the two types of arthritis:
They have similar symptoms and both affect the joints, but the origins are different.
While OA is usually an age-related condition caused by the wear and tear of joints, RA develops any time in life and is considered an auto-immune condition.
Osteoarthritis: New Medical Findings
Traditionally, OA was considered a non-inflammatory type of arthritis. However, new scientific findings suggest that in both cases, low-grade inflammation is a major driver of ongoing joint degeneration, and that the distinction might not be as big as once thought. Therefore, the diet recommendations described below can often refer to both types of arthritis.
Before implementing any (drastic) dietary changes, discuss it with your medical team.
Arthritis and Your Diet: The Connection (Based on Medical Studies)
A medical study found that nearly one-quarter of people with rheumatoid arthritis (RA) reported that diet had an effect on their RA symptoms.
To fight arthritis symptoms, it is generally recommended to eat a balanced diet, maintain a healthy body weight and reduce your stress levels.
According to Arthritis Research UK, some studies show that people who eat a lot of red meat are more likely to develop joint inflammation.
One medical study has also suggested that vegetarian and vegan diets can reduce the risk of rheumatoid arthritis. If you do follow such diets, you just need to make sure you provide your body with sufficient amount of nutrients from plant sources.
The most common nutritional deficiencies in vegetarians and vegans include:
- Calcium – check out these sources of calcium that are better than dairy products
- Selenium – try to eat a lot of nuts (especially Brazil nuts)
- Vitamin B12 – read my post about the warning symptoms of B12 deficiency
- Vitamin D – read my post about the 12 common diseases cause by vitamin D deficiency
If you think you might not be getting enough of these nutrients with your daily diet, consider a good quality supplement.
Foods to Eat to Fight Arthritis (Based on Scientific Studies)
1. Fish rich in omega-3 fatty acids
Research suggests that consumption of omega-3 fatty acids prevents inflammation.
A medical review of 20 randomized controlled trials reported that omega-3 fatty acids have some benefits on RA treatment. The scientific report also added that symptoms got worse in RA patients who discontinued the fish oil supplements.
Omega 3 fatty acids are readily available in oily fish, salmon being the prime example. Actually, all fish contain omega-3, so you needn’t limit yourself. The highest doses, however, are available in salmon, sardines, anchovies and herring. For example, a 3 ounce serving of salmon provides you with 2 grams of these healthy omega 3 fatty acids.
I’ve already mentioned the health benefits of omega 3 and the fact that consumption of oily fish can reduce the risk of breast cancer.
Taking omega 3 is also one of the 70 habits featured in my e-book 70 Powerful Habits For A Great Health which will guide you how to take positive steps to improve your wellness and overall health.
Plant sources of omega-3 are not as good
Unfortunately for vegetarians and vegans, plant sources of omega-3, such as flax seeds and walnuts, don’t contain a full spectrum of essential fatty acids. They contain only ALA (alpha-linolenic acid).
The body needs to convert the short-chain version (ALA) to a long-chain version (EPA and DHA) in order to make use of it, however some studies indicate that the conversion of ALA to DHA and EPA is relatively small.
Omega-6 to omega-3 ratio
Another important point I’ve written about before is the omega-6 to omega-3 ratio. The modern diet contains too much omega-6 and not enough omega-3 fatty acids.
The imbalance itself is often a cause of inflammation and needs to be addressed by increasing omega-3 intake and reducing omega-6. A scientific study mentioned that high omega 6 to omega 3 ratio may have adverse health effects. The same study adds that omega 6 fatty acids can be connected with inflammation.
Omega-6 fatty acids are present in vegetable oils, so are often consumed with the abundance of fried and processed goods we eat these days.
Your best bet to get it right is to increase fish consumption, and use oils that are low in omega-6, such as coconut oil and olive oil.
2. Extra-virgin olive oil
As I mentioned above, olive oil reduces your omega-6 intake and is a vital part of the Mediterranean diet, which has been linked to the reduction in RA symptoms.
Studies have shown that a compound in olive oil inhibits the production of chemicals that cause inflammation, which is very similar to the mechanism of pharmaceutical anti-inflammatory drugs. For more useful information about olive oil, read my post on how to use olive oil as a natural medicine.
3. Fruits and vegetables rich in antioxidants
Consuming food that contains a lot of antioxidants is another way to reduce your inflammation. Nutritionists often recommend eating colorful food – the reason for that is not esthetic, but health-related. Fruits and veg that are bright get their rainbow colors from flavonoids and carotenoids, which are powerful antioxidants. Checkout my post about the 5 reasons to eat multiple colored fruits & vegetables.
Fruits and veg high in antioxidants:
- Berries
- Broccoli
- Spinach
- Sweet potatoes
- Squash
- Carrots
- Tomatoes
- Melons
- Papaya
- Grapes
4. Whole grains
According to The American Journal of Clinical Nutrition, whole grains reduce inflammatory markers in the body and in this way prevent exacerbation of arthritis.
What about gluten and arthritis?
There is a concern that there is a link between gluten and aggravated symptoms of arthritis. The Arthritis Foundation wrote an article about “The Connection Between Gluten And Arthritis” in which the current recommendation is to avoid gluten if you have a gluten sensitivity or Celiac disease, but there is no general recommendation to avoid gluten if you suffer from arthritis but don’t suffer from gluten sensitivity or Celiac disease.
While the research is still debating about this point, bear in mind that not all whole grains contain gluten (like amaranth, buckwheat, millet, quinoa, oats, brown and purple rice and sorghum), and you can still include these in your diet.
5. Ginger
Ginger has been counted amongst the natural anti-inflammatory remedies. The study results have not been uniform, but, according to some reports, the root is supposed to act in a medicinal way and reduces inflammation.
Ginger is also one of the ingredients in my ultimate anti inflammatory smoothie and in my anti inflammatory turmeric ginger tea.
You can get more information about ginger in my post on how to use ginger as a natural medicine.
6. Turmeric (curcumin)
I wrote in the past about the amazing health benefits of turmeric. Curcumin, the component which gives turmeric its golden color and its many health benefits, has been well-studied over the years. It works as a powerful antioxidant and has anti-inflammatory and antiseptic properties.
One scientific study concluded that curcumin significantly slows OA disease progression.
A medical review of studies recommends the use of curcumin for many forms of arthritis and possibly other inflammatory conditions.
Turmeric is used in Traditional Chinese Medicine (TCM) and Indian Ayurvedic medicine to treat arthritis. It is claimed that turmeric reduces arthritis joint pain, inflammation, and stiffness related to arthritis.
Turmeric is also one of the superfoods mentioned in my e-book about superfoods which is part of the Natural Health Revolution Program. This program will help you to achieve your health, nutrition and weight loss goals.
7. Vitamin C
Vitamin C also works as an antioxidant and has been shown to reduce the risk of developing RA. Good sources of vitamin C include:
Berries are especially high in vitamin C and you can find easy and nutritious berry recipes in my e-book The Healing Berry Guide. This e-book will teach you how to transform your health with berries and their amazing health benefits.
You should stick with dietary sources of vitamin C, as big doses of supplements have been linked to arthritis flare-ups.
8. Virgin coconut oil can reduce inflammation
It is known that virgin coconut oil has anti-inflammatory properties, and the Arthritis Foundation has acknowledged it in their website.
In a study published in International Immunopharmacology the researchers extracted antioxidants unique to virgin coconut oil and injected them into rats with induced arthritis. They found that the unique coconut oil antioxidants reduced inflammation associated with arthritis more effectively than current pharmaceutical drugs.
You can consume virgin coconut oil in moderation, up to 2 tablespoons a day for an adult. However, don’t start immediately from 2 tablespoons a day, as it may cause you loose stools and nausea that may occur when consuming high amount of coconut oil. Start from 1 teaspoon per day, and gradually increase it to 2 tablespoons per day over 1 or 2 weeks.
Foods to Avoid if You Have Arthritis (Based on Medical Studies)
- Sugar – sugar consumption provides you with nothing but empty calories and increase your glucose levels. This has a negative impact on inflammation development and your overall health. One medical study found that regular consumption of sugar-sweetened soda, is associated with increased risk of RA in women.
- Trans fats – these fats are most common in processed foods and their consumption could cause inflammation. Try to avoid processed foods as much as possible.
- Red meat – excessive consumption of red meat has been linked to inflammatory reaction.
- Salt and sodium – you often consume salt without even realizing – it’s present in processed foods many people like to munch on. Overdoing it on salt can bring your blood pressure up – another risk factor for many chronic diseases. A review of medical studies found that “High sodium intake may be associated with a diagnosis of rheumatoid arthritis.”
Supplements for Treating Arthritis
Glucosamine can be effective for treating joint pain
Glucosamine reduces the symptoms of pain, swelling and stiffness of the joints. It is naturally synthesized in our body and present in our connective tissues such as the cartilage in our knees. As we age, we lose the amount of this substance in our body, which leads to thinning of cartilage, and that might progress to osteoarthritis.
Glucosamine cannot regenerate cartilage, but it can prevent further loss and stop the progression of arthritis. The good thing about it is that it doesn’t have serious side effects.
One scientific study in adults with osteoarthritis found that taking 1,500 mg of glucosamine daily for half a year reduced pain and improved function more than a placebo.
Another two scientific studies, showed that taking 1,500 mg of glucosamine sulfate daily for three years improved symptoms of osteoarthritis. One of the studies concluded that: “Long-term treatment with glucosamine sulfate retarded the progression of knee osteoarthritis”. The other study concluded that taking glucosamine can be good for treating symptoms of osteoarthritis.
Related: Scientifically Proven Natural Remedies For Knee Osteoarthritis (Evidence Based)
Chondroitin
Chondroitin is another building block of the connective tissue in our body. Its role is to stimulate the cartilage cells, and therefore works well with glucosamine to improve regeneration and recovery of the tissues.
It is recommended to take chondroitin together with glucosamine, as taking these two substances alone doesn’t seem to do very much. The effect of taking glucosamine and chondroitin takes about 8-12 weeks until you see results. The recommended dose is 1,500 mg of glucosamine sulfate a day in divided doses, and 800-1,500 mg of chondroitin sulfate. If you are allergic to sulfate, use hydrochloride version.
A review of medical studies concluded that chondroitin (alone or in combination with glucosamine) can improve pain in people with osteoarthritis.
Shea nut oil
Shea nut oil has natural plant components that are anti inflammatory. A recent study found that taking shea nut oil decreases significantly the inflammation and cartilage degeneration. Take as directed in the label.
One medical study found that shea nut oil can relieve the symptoms of knee osteoarthritis and can improve muscle control of the knee.
Safflower capsules
The benefits of safflower are relatively new to the West, but this plant has a centuries-old tradition of medicinal use in Asia.
One medical study mentioned that safflower is used to treat arthritis, and it has properties that reduce pain and inflammation. You can purchase it as a supplement (like this one)
MSM
MSM (methylsulfonylmethane) is a naturally occurring sulfur compound found in fresh fruits and vegetables, milk, fish, and grains. It is marketed as a dietary supplement for pain and inflammation associated with osteoarthritis. Recommended dose is 1,000 to 4,000 mg daily.
MSM benefits are based on testimonials but little valid scientific data. Although there is great interest in using MSM to treat a variety of conditions, including arthritis, more research is needed to determine its benefits and risks.
Vitamin D Deficiency and Rheumatoid Arthritis
Vitamin D is important for a good overall health and plays an important role in making sure our muscles, heart, lungs and brain function well. Our body can make its own vitamin D from sunlight.
Vitamin D deficiency is more common than you may think. In fact, The American Journal of Clinical Nutrition called it a worldwide problem which is recognized as a pandemic. I’ve already mentioned the importance of vitamin D and how it can cause 12 common diseases as well as dementia.
People who have higher levels of Vitamin D in their bodies have been found to have lower incidences of heart disease, depression, obesity and certain forms of cancers.
The Connection Between Vitamin D and Rheumatoid Arthritis (According to Science)
Medical study #1: vitamin D deficiency is linked to rheumatoid arthritis
A study published in the medical journal Endocrinology and Metabolism has found that vitamin D levels are significantly associated with disease activity, levels of inflammatory cytokines (small proteins), and bone loss in patients with rheumatoid arthritis.
According to the study, “it appears that vitamin D deficiency is highly prevalent in patients with rheumatoid arthritis, and that vitamin D deficiency may be linked to disease severity in rheumatoid arthritis”.
Scientists, doctors and researchers do not have a definitive answer as to why vitamin D plays an important role in the body (except for helping calcium metabolism). But they do know that the studies that have been done strongly suggest it’s better to not let it get too low in your body, especially if you suffer from rheumatoid arthritis.
Medical study #2: low levels of vitamin D can increase the risk of rheumatoid arthritis
A study conducted by researchers from Boston University and published in in the journal Environmental Health Perspectives took the connection between low levels of vitamin D and increased levels of rheumatoid arthritis activity one step further.
I have mentioned that vitamin D is naturally produced by our bodies when the sun’s UV rays shine upon our skin, so it would make sense that people who lived in warmer climates would get more sun and would have more vitamin D produced by their bodies naturally.
The Boston University researchers concluded that the percentage of people that reported having symptoms of rheumatoid arthritis in the north-eastern part of the USA, where they get less exposure to sun than other parts of the country, was much higher than those percentages of people that lived in so called ‘sunshine states’.
The lead researcher, Dr. Verónica Vieira, MS, had this to conclude: “Women in states like Vermont, New Hampshire and Southern Maine were more likely to report being diagnosed with rheumatoid arthritis”.
There’s higher risk in the northern latitudes and this might be related to the fact that there’s less sunlight in these areas, which results in a vitamin D deficiency.
How to Increase Your Vitamin D Levels
If you are an arthritis sufferer, then the next logical question is how do you increase the level of vitamin D in your body?
1. Get Some Sun
The first answer to this question would be to get more sun. A caucasian person at midday can get all the vitamin D their body needs in a day in less time than it takes for the skin to turn pink. It is also known that people with darker skin have more trouble absorbing the sun’s rays and subsequently producing vitamin D. Not to mention that too much sun can wrinkle your skin prematurely and cause skin cancer.
The more skin you expose the more vitamin D that your body produces. Just remember you might not want to bare it all because there are some spots on your body that will burn easily because they are not used to exposure.
This is not so difficult if you live in a warmer climate but if you live in a place which does not get much sun, as the second study suggested, then this may not be possible.
2. Consume Foods That are Naturally Rich in Vitamin D
If you don’t live in a warm climate then what do you do?
The next thing to try is adding foods that are rich in vitamin D to your diet. The daily recommended dose of vitamin D is 400 – 600 IU per day, but some nutritionists feel that up to 4000 units a day is needed for patients that suffer from rheumatoid arthritis. But make sure to consult with your doctor first.
3. Take vitamin D supplements
If all else fails then take an over the counter supplement. Most daily vitamin capsules contain a day’s recommended dosage of vitamin D. There are also supplements that contain much higher doses of vitamin D too.
Ask your doctor about these before you take them to see if they are safe for you to use.
If you suffer from rheumatoid arthritis, this low vitamin D level and arthritis connection is certainly worth keeping an eye on. Millions of people around the world suffer from rheumatoid arthritis and there will surely be new studies results coming out in the very near future.
Here are some suggestions:
- Cod Liver Oil (you can get it packed in capsules – like this one or in a bottle like this one)
- Oily Fish (Salmon, Tuna)
- Portobello Mushrooms
- Extra Lean Ham
- Hard Boiled Eggs
Related articles:
